Today, May 2, the National Institutes of Health (NIH) recognizes World Asthma Day and the innovative research that is helping to shed light on the disease, pave the way for effective treatments, and improve the lives of people who have asthma.
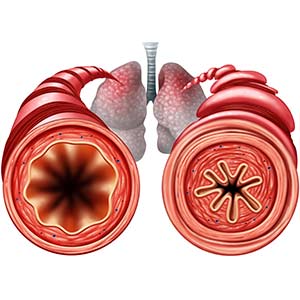
In the United States alone, more than 25 million individuals — including more than 4 million children — experience asthma, which is a chronic lung disease that can cause coughing, wheezing, chest tightness, and shortness of breath. In severe cases, breathing becomes extremely difficult, and it feels like a weight compresses the chest. Worsening asthma can lead to missed time at school and work, emergency room visits, and even death.
Several NIH institutes conduct and support asthma-related research, including the National Institute of Environmental Health Sciences (NIEHS); the National Heart, Lung, and Blood Institute (NHLBI); and the National Institute of Allergy and Infectious Diseases (NIAID). Each year, they come together to reaffirm the NIH commitment to studying asthma and enhancing patient care in the United States and globally.
During the past year, NIH scientists and grant recipients advanced groundbreaking research that opens doors for new treatments and interventions, addresses disparities in asthma-related health outcomes, and expands our understanding of this chronic respiratory disease.
Understanding who is at risk, and why
NIEHS researchers discovered that frequent wood burning at home is linked to decreased lung function in adults with asthma. Many people in rural parts of the United States (and many individuals in other countries) burn wood and other biomass indoors for cooking and heating. People with asthma should consider reducing indoor wood burning or using air filtration devices, according to the scientists.
Other NIEHS researchers found that following the 2010 Deepwater Horizon disaster, oil spill cleanup workers — many of whom were exposed to airborne contaminants, such as petroleum hydrocarbons — experienced increased risk of asthma. In the largest-ever study of its kind, the scientists analyzed data from nearly 25,000 cleanup workers and 8,000 nonworkers. The researchers showed that cleanup workers had a greater chance of developing asthma in the three years following the oil spill compared with nonworkers.
NIAID-funded scientists found that increased levels of two outdoor air pollutants — ozone and fine particulate matter — are associated with non-viral asthma attacks in children and adolescents who live in low-income urban areas. The study also identified associations between exposure to the two pollutants and molecular changes in the children’s airways during non-viral asthma attacks, suggesting potential biological mechanisms involved in such attacks.
Other NIAID-supported researchers discovered that the absence of a respiratory syncytial virus (RSV) infection in children before their first birthday is associated with a 26% lower risk of developing childhood asthma. RSV is the most common cause of severe lung disease in children younger than age one year in the United States. The finding represents additional evidence for a link between RSV infection in infancy and higher incidence of asthma at age five years. This evidence supports a need to study long-term respiratory outcomes among children in clinical trials of RSV prevention products such as vaccines.
Research lays foundation for improved treatments
Through the NHLBI-funded Severe Asthma Research Program, scientists are beginning to understand how asthma and obesity — conditions that often occur in the same people — might be related. Obesity can cause resistance to insulin, which is a hormone that controls blood sugar levels, and such resistance has been linked to asthma risk in adults.
In a related NHLBI-funded study in people with severe asthma, scientists found that those with moderate or severe insulin resistance had lower lung function and did not respond as well to asthma treatment (steroids or bronchodilators). More clinical trials are needed to test whether treatments for insulin resistance can help prevent accelerated loss of lung function due to asthma, according to the researchers.
Elsewhere, NIEHS grant recipients conducted a study in mice involving agricultural dust exposures, and they uncovered a novel role for the protein IL-22 in lung repair. Their findings could aid development of therapeutics for farmworkers and others experiencing environmentally induced lung diseases, such as asthma.
Reducing asthma attacks in disadvantaged youth
NIAID-supported researchers found that the monoclonal antibody mepolizumab decreased asthma attacks by 27% in Black and Hispanic children and adolescents who had a form of severe asthma, were prone to asthma attacks, and lived in low-income urban neighborhoods. This population has been underrepresented in previous clinical trials of asthma therapeutics.
An analysis of gene activity in cells collected from study participants’ nasal secretions showed that mepolizumab tamped down the activity of three gene networks associated with allergic airway inflammation and asthma attacks but did not reduce the activity of six other networks related to tissue inflammation and mucus overproduction. These findings pave the way for using gene activation patterns to monitor new asthma therapies in future clinical trials involving this study population.
Also, NIAID launched a clinical trial to test whether a different monoclonal antibody, dupilumab, can reduce asthma attacks and improve lung function in children with poorly controlled allergic asthma who live in low-income urban neighborhoods. Dupilumab is approved by the U.S. Food and Drug Administration as an add-on maintenance treatment for certain types of moderate-to-severe asthma in people aged 6 years and older. However, little data exist on the effectiveness of the drug in Black and Hispanic children, even though severe asthma disproportionately affects U.S. children in those groups. The NIAID study will help fill this knowledge gap.
Addressing disparities through collaboration
In 2017, NHLBI launched a research program to improve asthma care for children on the Navajo Nation, which is the largest and most populous tribal reservation in the United States. Children on Navajo Nation are disproportionately affected by asthma. Due to the COVID-19 pandemic, scientists have only recently been able to return to the reservation, but the partnerships and training provided to tribal communities helped to maintain the program during the past few years. The initiative helps to increase access to asthma medication and education in schools, and to expand health-care provider training in asthma care. Details of the program are described in a 2022 journal article.
Also, a school-based program that has demonstrated success in addressing asthma among disadvantaged youth in the Denver metropolitan area will be expanded to include five other regions of Colorado, including midsize cities and rural areas. Investigators leading these efforts are part of an NHLBI-supported alliance called DECIPHeR (Disparities Elimination through Coordinated Interventions to Prevent and Control Heart and Lung Disease Risk), which aims to engage with community stakeholders, understand their needs, and improve health outcomes.
Zero-emissions vehicles reduce emergency room visits
NIEHS-funded scientists and their colleagues analyzed data on adoption of zero-emissions vehicles (ZEVs) in California and discovered an accompanying reduction in air pollution levels and asthma-related emergency room visits. ZEVs include battery electric, plug-in hybrid, and hydrogen fuel cell cars. The researchers identified a 3.2% drop in asthma-related emergency visits and a small reduction in nitrogen dioxide for every additional 20 ZEVs per 1,000 people.
ZEVs may help to mitigate climate change and reduce health disparities in low-income neighborhoods, according to the researchers.
Other NIEHS-funded researchers analyzed New York City’s Clean Fuel Bus Program from 2009 to 2014 and found that it led to significant reductions in concentrations of air pollutants that can contribute to asthma.