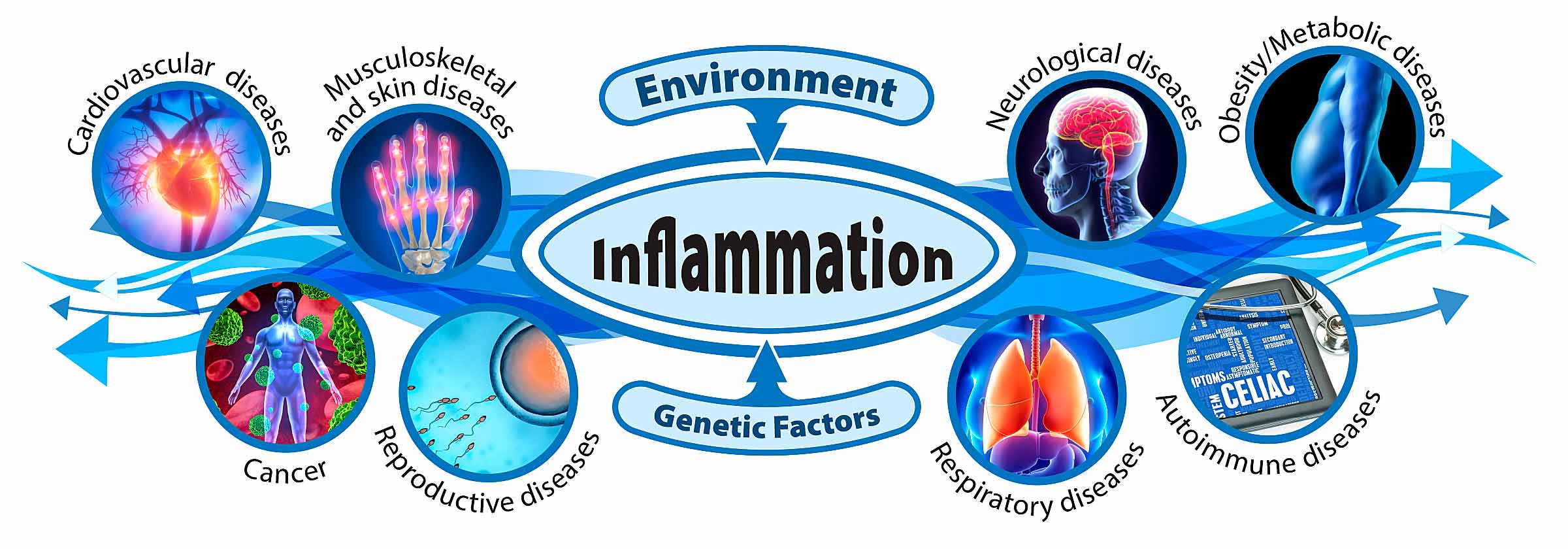
A new paper highlights the toll on life and health from chronic inflammatory diseases, which are at the root of more than half the deaths worldwide, according to its authors. New research is needed to reduce that toll.
 Kleinstreuer is the deputy director of the NTP Interagency Center for the Evaluation of Alternative Toxicology Methods. (Photo courtesy of Steve McCaw)
Kleinstreuer is the deputy director of the NTP Interagency Center for the Evaluation of Alternative Toxicology Methods. (Photo courtesy of Steve McCaw)National Toxicology Program (NTP) scientist Nicole Kleinstreuer, Ph.D.; NIEHS grantee Gary Miller, Ph.D., from Columbia University; and National Institute on Aging Scientific Director Luigi Ferruci, M.D., Ph.D., were co-authors of the review, published Dec. 5 in Nature Medicine.
The two faces of inflammation
The body’s immune system responds to threats, such as infection and injury, with a cascade of changes that lead to localized inflammation. Once disease-causing agents and tissue damage are resolved, the inflammatory state should also resolve.
The authors, led by David Furman, Ph.D., from Stanford University and Universidad Austral in Argentina, explained that a whole host of factors can result in a state called systemic chronic inflammation (SCI). This low-grade chronic state “is characterized by the activation of immune components that are often distinct from those engaged during the acute immune response,” the authors observed.
Biomarkers needed
Most well-known biomarkers of inflammation reflect acute reactive processes, so they are not considered good predictors of the chronic state, noted Kleinstreuer.
Inflammaging, for example, is a term for chronic inflammation that characterizes the aging process. “We have decent surrogates for understanding inflammaging and other processes associated with increased risk for cardiovascular disease and mortality,” she explained. “But there is a real lack of consistency across the population in the predictive power of specific molecules as biomarkers for SCI.”
Genetic diversity does not fully explain the lack of consistency. “It’s probably more driven by environmental and epigenetic factors than by hereditary components,” Kleinstreuer suggested.
Cleaning up the mess
The complexity of the biological pathways involved is another challenge researchers face. In March, NIEHS hosted a workshop focused specifically on how the body resolves inflammation.
“Understanding whether SCI is an outcome of changes in inflammation resolution pathways is critical,” said Sri Nadadur, Ph.D., the workshop’s lead organizer. “This knowledge will help clarify how factors as different as exposure to environmental toxicants, and physical activity or lack of it, may worsen asthma, obesity, and other health outcomes that have underlying SCI conditions.”
Social, environmental, lifestyle risk factors
The review found themes among studies of both the onset and resolution of inflammation. Some are listed below.
- Physical activity — When skeletal muscles contract, they release proteins that can systematically reduce inflammation.
- Microbiome — Studies of various microbiome imbalances and disease states show connections to inflammation.
- Diet — Diets high in refined grains, alcohol, and ultra-processed foods can alter gut microbiota and lead to intestinal and immune changes.
- Social and cultural changes — Disrupted sleep patterns, psychosocial stress, artificial light, and other factors influence the immune system.
- Environmental and industrial toxicants — The federal Tox21 Program has demonstrated that chemicals we commonly encounter alter molecular signaling pathways that underlie inflammation.
- Developmental origins — Childhood obesity, psychological stress, microbial exposure in infancy, and prenatal conditions are linked to changes related to SCI, often through epigenetic changes.
Types of research needed
Finally, the authors called for new research directions to support early diagnosis, prevention, and treatment of SCI.
- Collect data on multiple factors that affect SCI by combining whole blood gene expression, analyses of certain cell types, and other approaches.
- Determine robust biomarkers that address not only inflammation, but anti-inflammatory pathways.
- Design studies to reveal biological reactivity and recovery from immune system challenges, to clarify sources of differences among individuals.
- Focus on modifiable factors that influence inflammation, such as activity, diet, toxicant exposures, and stress.
Citation: Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, Ferrucci L, Gilroy DW, Fasano A, Miller GW, Miller AH, Mantovani A, Weyand CM, Barzilai N, Goronzy JJ, Rando TA, Effros RB, Lucia A, Kleinstreuer N, Slavich GM. 2019. Chronic inflammation in the etiology of disease across the life span. Nat Med 25(12):1822–1832.