How the body repairs DNA damage following exposure to a chemical called N-nitrosodimethylamine (NDMA) can provide new insights for cancer treatment, according to Jennifer Kay, Ph.D. The former NIEHS Superfund Research Program (SRP) trainee presented her findings during the Aug. 1 Wetterhahn Award Seminar.

NDMA is a probable human carcinogen that contaminates the groundwater in Wilmington, Massachusetts, due to ineffective containment of millions of gallons of hazardous waste at the Olin Chemical Superfund site. Although the site closed in 1986, the plume of contaminants has migrated far beyond the site itself.
“NDMA is not just a concern at Superfund sites — it’s also a byproduct of drinking water disinfection and has recently been found to contaminate common drugs, such as blood pressure medications, sometimes in very high levels,” Kay said. “Millions of people have been exposed to NDMA and may face serious health consequences.”
Cancer-causing pathways
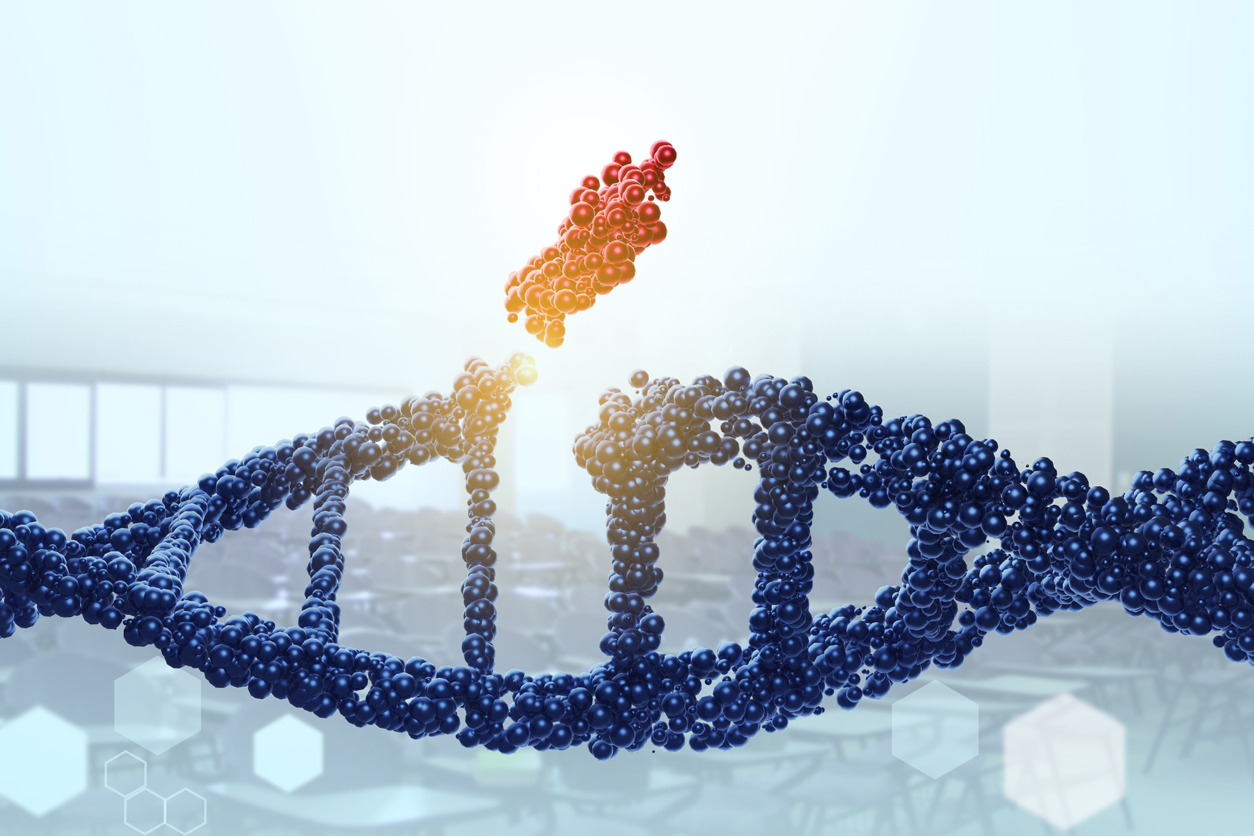
NDMA is metabolized in the liver into a reactive form that can harm DNA. Kay’s research focuses on a specific type of DNA damage that blocks replication, which is an essential process for making copies of the DNA double-helix in cells. Inability to accurately replicate DNA can lead to mutations and eventually cancer.
Cells have sophisticated DNA repair systems to fix damage that blocks replication. For example, during the base excision repair process, the enzyme AAG snips off the damaged portion of the DNA called a base. Two bases form a base pair, which looks like a ladder rung between DNA’s two strands that wind around each other like a twisted ladder. Other enzymes recognize the gap resulting from the missing base and create a nick in the DNA strand, specifically its phosphate backbone. The gap is then filled, and the remaining nick sealed.
“One unfortunate problem with base excision repair is that it breaks the DNA strand as part of the repair process,” Kay said. “If the cell tries to replicate its DNA while there are nicks in the backbone, the strands of DNA that are getting replicated could fall apart, causing mutations or cell death.”
Enzymes and cancer treatments
Kay led a study that examined how mice with different AAG enzyme levels responded to NDMA exposures.
After receiving a high dose of NDMA, mice that were genetically modified to overexpress AAG tended to accumulate lots of DNA breaks. The reason: The rest of the repair machinery could not keep up with sealing all the breaks in the backbone. Mice that lacked AAG enzymes had more mutations because they were unable to repair the damage following NDMA exposure.
“Interestingly, too much AAG was actually more lethal than a lack of AAG, because all the breaks in the DNA were too toxic for the cells to survive,” Kay explained. “However, mice lacking AAG had more mutations and cancer later in life.”
According to Kay, a balanced repair pathway — just the right amount of AAG — is essential for disease-free survival.
AAG enzyme activity can naturally vary from person to person by as much as 2,000%, which may be key to creating personalized cancer therapies, Kay noted.
“Screening for AAG activity in humans could allow us to identify people exposed to NDMA who may be at a greater risk of developing cancer,” Kay said. “Many other chemicals, including both environmental exposures and chemotherapeutics, also cause replication-blocking damage. This could help inform studies of both cancer treatment and prevention.”
Examining estrogen disruptors
At Silent Spring Institute, Kay now studies the interactions between DNA damage and the body's hormone function, focusing specifically on chemicals that increase estrogen signaling. Excess estrogen can promote cancer development by stimulating cell division, causing existing mutant cells to proliferate.
Exposure to chemicals that damage DNA and that activate estrogen signaling likely increases breast cancer risk more than either alone, because cells that try to divide when they have unrepaired DNA damage are more likely to get mutations.
“I hope to understand the pathways behind how these chemicals cause breast cancer and create a platform to identify potential carcinogens more efficiently,” Kay said.
Kay, who received the 2020 Karen Wetterhahn Memorial Award, credits her work with SRP as driving her goal to expand the world of cancer research to better represent an array of environmental exposures.
(Lauren Sprouse is a science communication specialist for MDB, Inc., a contractor for the NIEHS Superfund Research Program.)