Before the advent of recent treatments, the autoimmune muscle disease known as myositis was deadly. Of the patients who did survive, many were severely physically disabled.
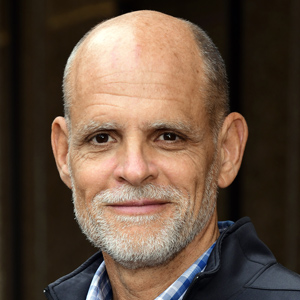
Rare diseases like myositis are often challenging to study and treat because the smaller number of cases makes it difficult to draw scientific conclusions. However, Lisa Rider, M.D., a pediatric rheumatologist who leads the NIEHS Environmental Autoimmunity Group, has been at the forefront of collaborations to identify genetic and environmental risk factors for myositis in children, classify patients’ symptoms, and uncover cellular markers of disease progression and treatment response. In addition, her work to measure how patients respond to therapies led to the successful development of the first Food and Drug Administration-licensed product to treat myositis in several decades.
“As a world leader in pediatric rheumatology and the myositis syndromes, Dr. Rider’s seminal research has substantially contributed to our understanding of how autoimmune muscle diseases develop, can be divided into mutually distinct phenotypes, and how they are best assessed and treated,” the Association of American Physicians (AAP) wrote in announcing Rider’s selection to the elite honorary medical society.
Rider was inducted into the prestigious organization during an awards ceremony April 6 in Chicago. Founded in the 1800s, AAP membership is limited to physicians who are also scientists who have made impactful research contributions to advance biomedical science, medicine, or health.
“The fact that AAP is a national society and only has about 1,800 active members across the country and all disciplines of medicine — including pediatrics, surgery, OB-GYN, and psychiatry — is a real testament of the honor of becoming a new member,” said NIEHS Clinical Director Janet Hall, M.D. “It is highly competitive.”

Many Nobel laureates and members of the National Academy of Sciences and the National Academy of Medicine have been inducted into the organization.
“It is a tremendous honor to have my work recognized as having that much impact on the field,” said Rider. “I would like to deeply thank all the members of our team, our trainees and collaborators, and our patients for all their contributions to the work. I particularly thank Fred Miller, with whom I worked closely for several decades, and his partnership in much of this work. The honor speaks volumes to our great team that has been able to do this fantastic research and for it to be recognized in this way.”
A leader in diagnosing patients
Myositis, which occurs when the immune system goes awry and attacks healthy muscles and other tissues, affects approximately 75,000 people in the U.S. each year. Although the disease is considered rare, it may be underdiagnosed, with recent reports of some forms of myositis in children being mistaken for muscular dystrophy.
Although symptoms vary among patients with the disease, children with the most common form of myositis — known as juvenile dermatomyositis — often present with characteristic rashes on the eyelids or over the knuckles, elbows, or knees. According to Rider, patients also can have photosensitive rashes, which are rashes brought on by exposure to sunlight. Muscle weakness close to the center of the body and in the shoulders or hip girdle is another common symptom. This muscle weakness can make it difficult to climb stairs, get into a car, pick things up, get out of bed, or shampoo hair.

“These are systemic autoimmune diseases, meaning the body’s immune system can mistakenly attack other parts of the body, such as the lungs, heart, and GI tract,” Rider explained. “There can be difficulty swallowing and arthritis is a very common feature.”
Understanding how the disease presents differently and linking those symptoms to the presence of specific autoantibodies allowed Rider and her team to identify distinct subgroups of patients. Unlike antibodies generated by a healthy immune system to fight viruses, autoantibodies attack substances made by a person’s own body and are a hallmark of autoimmune diseases.
Thanks to Rider’s discovery of the anti-TIF1-gamma autoantibody, in collaboration with Ira Targoff, M.D., and colleagues, clinicians around the world can now order blood tests to look for specific autoantibodies present in their patients. These autoantibodies can indicate whether a patient’s health outcomes will be more or less severe.
New treatments, thanks to research
Early clinical trials of new therapies to treat myositis failed because of an inability to uniformly determine which patients exhibited clinical improvement. To develop the response criteria for assessing improvement, Rider and her team first created a national registry to pool patient data. They characterized participating patients across North America in terms of their demographics, environmental exposures, clinical features, responses to treatments, and disease outcomes.
Because of Rider’s work, validated tools to assess disease activity and damage, and how they change over time in response to treatment, exist today. This scoring system, developed by Rider and long-time NIEHS collaborator Frederick Miller, M.D., Ph.D., through the International Myositis Assessment and Clinical Studies Group, is now widely used in clinics and endorsed by the American College of Rheumatology and European Alliance of Associations for Rheumatology.
Omics discoveries on the horizon

Rider’s research to assess gene and protein regulation in children and adults with dermatomyositis is helping to identify new pathways that may be targeted for therapy. Her recent study — which uniquely analyzed RNA transcripts and protein expression together and increased the identification of pathogenic pathways — was recognized by NIEHS leaders as a 2023 Paper of the Year.
In addition, Rider recently received funding to evaluate how the levels of chemicals and other environmental exposures differ between identical twins and close-in-age same-gender siblings, specifically when one twin or sibling has an autoimmune disease and the other does not.
Because identical twins and siblings are more genetically similar, the goal is to tease out the role different environmental exposures play in myositis by measuring the levels of certain chemicals called metabolites in the blood. The researchers will cast a broad net to capture the totality of environmental exposures and the body’s response to them (exposomics). They also will look for the presence of specific chemicals such as PFAS, or perfluoroalkyl and polyfluoroalkyl substances.
“Dr. Rider’s work is a wonderful example of our investment in physician-led science to transform understanding of a rare disease, and translate that knowledge to improve patients’ lives,” said NIEHS Scientific Director Darryl Zeldin, M.D. “Being inducted into the AAP is a very big honor and reflects the sustained, impactful, and innovative science Dr. Rider has contributed to the field.”
(Caroline Stetler is Editor-in-Chief of the Environmental Factor, produced monthly by the NIEHS Office of Communications and Public Liaison.)