Inhaling unfragmented hyaluronan improved lung function in patients suffering from severe episodes of chronic obstructive pulmonary disease (COPD), according to NIEHS researchers and their collaborators.
Hyaluronan, a sugar secreted by living tissue that acts as a scaffold for cells, is also added to cosmetics as a skin moisturizer and nasal spray to moisturize lung airways. Used as a treatment, hyaluronan shortened the amount of time COPD patients in intensive care needed breathing support, shortened their hospital stay, and lowered medical costs.
Based on pollution research
 'Our goal was to get these patients out of intensive care and prevent them from being put on a ventilator,' Garantziotis said. (Photo courtesy of Steve McCaw / NIEHS)
'Our goal was to get these patients out of intensive care and prevent them from being put on a ventilator,' Garantziotis said. (Photo courtesy of Steve McCaw / NIEHS)The study, published Feb. 1 in the journal Respiratory Research, is a good example of how examining the impacts of environmental pollution on the lungs can lead to viable treatments.
Several years ago, co-senior author Stavros Garantziotis, M.D., medical director of the NIEHS Clinical Research Unit and head of the Matrix Biology Group, showed that exposure to pollution causes hyaluronan in the lungs of mice to break apart into fragments. These fragments irritate lung tissue and activate the immune system, leading to airway constriction and inflammation.
He determined that inhalation of healthy, unfragmented hyaluronan reduced inflammation by outcompeting the hyaluronan fragments.
Garantziotis offered an analogy for how the inflammation occurs. Hyaluronan surrounds cells like mortar surrounds bricks, he said. Introducing pollution causes cracks in the mortar, breaking it into smaller chunks.
'These smaller chunks irritate the body and activate the immune system, leading to inflammation,' Garantziotis said. 'Reintroducing the full-length hyaluronan, like a fresh coat of mortar, means it is less irritating and reduces the amount of inflammation.'
Patients see significant improvement
Because hyaluronan was approved in Italy for airway moisturization, Garantziotis worked with colleagues in Rome to see if inhalation of full-size hyaluronan could improve lung function in critically ill COPD patients. The patients used a breathing apparatus similar to a continuous positive airway pressure (CPAP) machine to treat dangerous episodes of worsened COPD, called acute exacerbation. This apparatus provided breathing support by blowing air into the airways through a mask.
“Inhaled hyaluronan qualifies as a stimulating aid for patients with exacerbated COPD, as it is safe and easy to administer,” said co-senior author Raffaele Incalzi, M.D., from Campus Bio-Medico University and Teaching Hospital in Rome. “Furthermore, it acts locally, only in the bronchial tree, and, thus, cannot interfere with any systemic drug.”
Mucus flow implicated
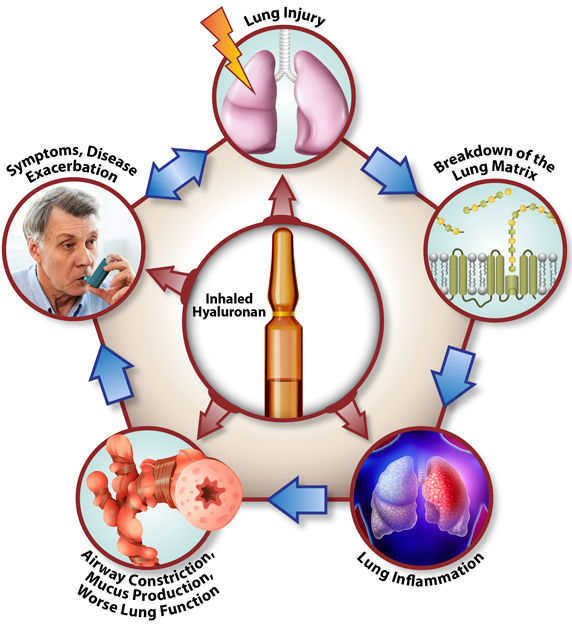 In the new study, inhaling hyaluronan interfered at almost every step of the COPD cycle, potentially making it a potent treatment for chronic lung disease. (Illustration courtesy of Stavros Garantziotis / NIEHS)
In the new study, inhaling hyaluronan interfered at almost every step of the COPD cycle, potentially making it a potent treatment for chronic lung disease. (Illustration courtesy of Stavros Garantziotis / NIEHS) Garantziotis also wanted to know what caused airway constriction in the lungs of COPD patients. He theorized that thick mucus may be involved.
Collaborating with scientists at the University of Alabama at Birmingham (UAB), they grew airway cells from emphysema patients and looked at how mucus moved in the cells. They saw that mucus flowed more easily after administering hyaluronan.
Co-author Steven Rowe, M.D., director of the Gregory Fleming James Cystic Fibrosis Research Center at UAB, said if patients with severe COPD took hyaluronan, the treatment would improve mucus transport and aid their recovery.
Future studies in U.S.
Current treatments for lung disease include inhaled steroids, antibiotics, and bronchodilators, so using a molecule that is already found in the body is a new concept.
The goal now for Garantziotis is to study this treatment in more patients in the U.S., so he can understand the optimal conditions and dosing that will produce the most benefit.
Citations:
Galdi F, Pedone C, McGee CA, George M, Rice AB, Hussain SS, Vijaykumar K, Boitet ER, Tearney GJ, McGrath JA, Brown AR, Rowe SM, Incalzi RA, Garantziotis S. 2021. Inhaled high molecular weight hyaluronan ameliorates respiratory failure in acute COPD exacerbation: a pilot study. Respir Res 22(1):30.
Garantziotis S, Li Z, Potts EN, Kimata K, Zhuo L, Morgan DL, Savani RC, Noble PW, Foster WM, Schwartz DA, Hollingsworth JW. 2009. Hyaluronan mediates ozone-induced airway hyperresponsiveness in mice. J Biol Chem 284(17):11309–11317.









