 One major goal of Wade’s lab is to understand how environmental exposures alter gene activity via chemical modifications to DNA that do not involve changes in the DNA sequence. (Photo courtesy of Steve McCaw)
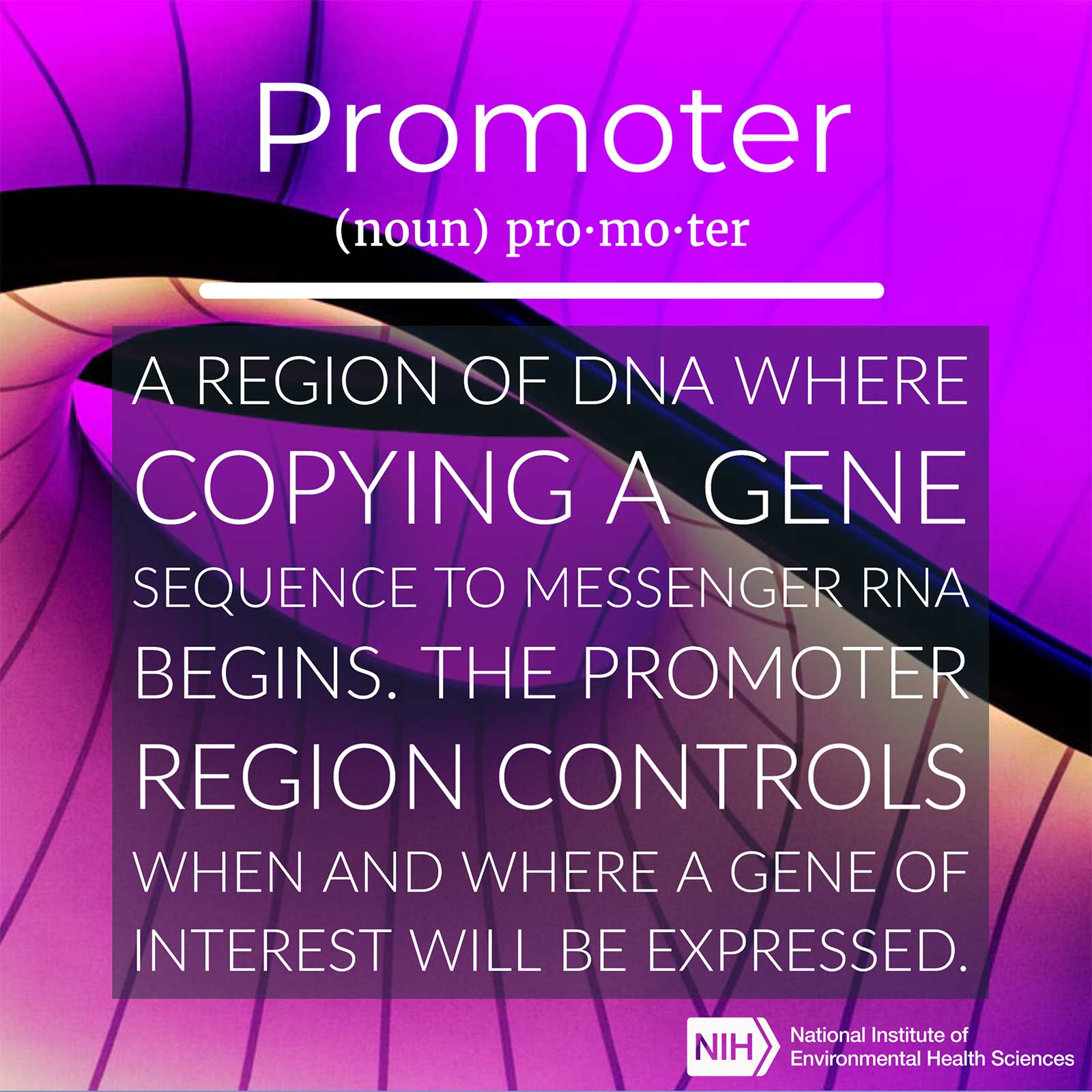
One major goal of Wade’s lab is to understand how environmental exposures alter gene activity via chemical modifications to DNA that do not involve changes in the DNA sequence. (Photo courtesy of Steve McCaw)New insights into how the liver adapts to a high-fat diet may lead to novel treatments for obesity-related diseases such as nonalcoholic fatty liver disease, according to a study by NIEHS researchers. They found that long-term consumption of a diet high in saturated fat led to dramatic reprogramming of gene regulation in the mouse liver. The study was published Feb. 19 in Nature Communications.
“We now have a detailed picture of molecular events that occur as the body adapts to diet with changes that lead to disease,” said senior study author Paul Wade, Ph.D., deputy chief of the NIEHS Epigenetics and Stem Cell Biology Laboratory. “One important outcome is the identification of regulatory DNA that control genes integral to diseases such as metabolic syndrome.”
Fat damages liver’s work
With the spread of high-fat diets and other elements of the Western lifestyle, obesity and related conditions are a growing health concern. For example, nonalcoholic fatty liver disease is now the most common chronic liver disorder in Western countries, according to the National Library of Medicine. In the United States, the condition affects between 30% and 40% of adults.
Nonalcoholic fatty liver disease involves the buildup of excessive fat in the liver of an individual who is not a heavy user of alcohol. Ultimately, this fat buildup may cause damage that affects the liver’s ability to break down food, store energy, and remove waste products.
“In a sense, nonalcoholic fatty liver disease and associated conditions can be considered an extreme case of metabolic adaptation to diet,” said first author Yufeng Qin, Ph.D., a postdoctoral fellow in the NIEHS Eukaryotic Transcriptional Regulation Group.
 Qin applied a relatively new technique called promoter capture Hi-C to examine long-range promoter-enhancer interactions. (Photo courtesy of Steve McCaw)
Qin applied a relatively new technique called promoter capture Hi-C to examine long-range promoter-enhancer interactions. (Photo courtesy of Steve McCaw)Regulation of genes altered
When too many calories are consumed, the liver adapts by reprogramming the regulation of gene activity. First, proteins called transcription factors bind to short regions of DNA called enhancers. The enhancers then interact with other short regions of DNA, called promoters, to make it more likely that a particular gene will be transcribed.
Promoters are typically next to the genes they regulate, in terms of the linear DNA sequence. Enhancers are usually located far away.
“This has made it difficult to accurately assign specific enhancers to their target genes,” said study author Sara Grimm, Ph.D., deputy director of the Integrative Bioinformatics Support Group at NIEHS. “As a result, it has not been entirely clear how gene regulatory networks in the liver adapt to excessive calorie intake.”
New method gets results
To help fill this knowledge gap, the researchers turned to a relatively new technique called promoter capture Hi-C. Researchers used this method to look across the whole genome and find long-range interactions between promoters and distant regulatory sites, such as enhancers.
The scientists fed mice a high-fat diet and used Hi-C and other techniques to analyze the effects on liver tissue (see sidebar). Not surprisingly, the mice became obese and showed other changes similar to metabolic syndrome in humans. Moreover, their livers became fatty and showed wide-ranging abnormalities at both molecular and cellular levels.
Changes in pre-wired pathways
 Before joining NIEHS, Grimm worked as a bioinformatics scientist at GlaxoSmithKline and as a research associate at the University of North Carolina at Chapel Hill. (Photo courtesy of Steve McCaw)
Before joining NIEHS, Grimm worked as a bioinformatics scientist at GlaxoSmithKline and as a research associate at the University of North Carolina at Chapel Hill. (Photo courtesy of Steve McCaw)The liver’s adaptation to the fat-rich diet was mediated by a transcription factor called hepatocyte nuclear factor 4 alpha (Hnf4-alpha). Notably, this transcription factor primarily uses promoter-enhancer loops that are already in place.
This finding suggested that Hnf4-alpha may play a central role in orchestrating changes in gene regulation in response to metabolic cues.
“Our results show that the changes in gene expression can occur through pre-wired molecular pathways, as opposed to newly generated pathways. The changes probably depend on the transcription factors that are activated by diet and obesity,” Wade said. “Further research on Hnf4-alpha and other important transcription factors could lead to potential therapies for patients with metabolic disease.”
Citations:
Qin Y, Grimm SA, Roberts JD, Chrysovergis K, Wade PA. 2020. Alterations in promoter interaction landscape and transcriptional network underlying metabolic adaptation to diet. Nat Commun 11(1):962.
Spengler EK, Loomba R. 2015. Recommendations for diagnosis, referral for liver biopsy, and treatment of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Mayo Clin Proc 90(9):1233–1246.
(Janelle Weaver, Ph.D., is a contract writer for the NIEHS Office of Communications and Public Liaison.)